Use this interactive to discover a range of resources about microorganisms and antimicrobial resistance. Select a label for more information.
Go here for further information, including the transcript.

This interactive diagram provides a selection of pathways that allow for different approaches and starting points using resources about microorganisms, the immune system and antimicrobial resistance. The aim is to assist educators with their planning of lessons and units of work by providing options that cover multiple science concepts. This interactive uses selected resources – additional resources are curated in our article Antimicrobial resistance explained.
The article Antimicrobial resistance – a context for learning provides pedagogical suggestions and links to the New Zealand Curriculum.
To use this interactive, move your mouse or finger over any of the labelled boxes and click to obtain more information.
Transcript
History of antibiotics
Before Alexander Fleming discovered penicillin, infections could lead to death, and common diseases such as pneumonia were fatal. During the First World War, one-third of soldiers died from infection or disease.
Penicillin – the first modern antibiotic – was discovered in 1928. The 1940s–1960s are considered ‘the golden age’ of antibiotics due to multiple antibiotic discoveries. However, soon after their discovery, bacteria started developing resistance, and the effectiveness of many antibiotics was reduced or even lost.
To compound this further, new antibiotic discovery has fallen away, meaning if we don’t use antibiotics carefully to reduce antibiotic resistance we may return to an age where infections are not readily treated and surgeries, including open-heart surgery or hip replacements, may be too dangerous to undertake.
The following resources provide information about the history of antibiotic discovery and resistance development.
Articles
- The history of antibiotics and antimicrobial resistance
- Antimicrobial resistance explained
- Fighting infection – timeline
- Resistance: When antibiotics don’t work – School Journal article
Media
- Antibiotics and antimicrobial resistance – a timeline – interactive timeline
- How bacteria develop resistance to antibiotics – video
Image: Professor Alexander Fleming, who first discovered the mould Penicillium notatum, at his laboratory in London (1943). Public Domain.
Protecting our future – slowing the spread
Preventing infection and controlling disease is one of the best actions we can take to slow the development of antibiotic resistance. Prevention can be achieved through measures such as vaccination, good hygiene and only using antibiotics when needed and as prescribed. These principles apply to people, pets and livestock.
Articles
- Reducing the risks of antimicrobial resistance
- Is the post-antibiotic era here now?
- Global report on antimicrobial resistance
- Antimicrobial resistance – a context for learning
- The environmental fate of chemicals – a context for learning
Media
- MPI antimicrobial resistance – for pet owners – YouTube video (Ministry for Primary Industries)
- Antimicrobial resistance – YouTube video (Food and Agriculture Organization of the United Nations)
- How to help slow the spread of antibiotic-resistant bacteria – video
Image: Illustration of antibiotic resistance in pets, Ministry for Primary Industries.
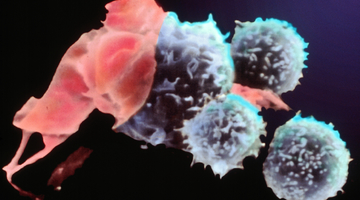
Immune system and treatments
The immune system consists of cells, tissues and organs that work together to protect us from infection.
Articles
- The immune system
- Vaccines and therapies
- The body’s first line of defence
- The body’s second line of defence
Activities
- The wars within
- Fighting infection card game
- Making snot
- Spreading diseases
- Fighting infection, the immune system – unit plan
Collection curations
Image: T helper cell response to virus infection.
Background – microorganisms
The main microorganisms in and on our bodies are protozoa, algae, fungi, bacteria and viruses. Most microorganisms are beneficial – for example, there are microorganisms in our large intestine that synthesise vitamins and allow them to be absorbed into the bloodstream. However, a tiny minority are pathogens. These pathogens, often called germs or bugs, are a threat to all life forms.
Articles
- Microorganisms – introduction
- Microorganisms – friend or foe?
- Fungi – the good, the bad and the ugly
- Bacteria – good, bad and ugly
- Bacteria
- Viruses
Activities
Image: Medical illustration of multidrug-resistant Pseudomonas aeruginosa bacteria, by Jennifer Oosthuizen for the CDC. Public domain.
AMR – mechanisms and spread
Any time antibiotics are used, they can contribute to antimicrobial resistance. Antimicrobial resistance is driven by a combination of exposure of bacteria to antibiotics, the spread of those resistant bacteria or the spread of the genes that code for resistance to other bacteria. If too many antibiotics are being used unnecessarily or misused, usefulness of these important drugs is threatened.
Everyone has a role to play in improving antibiotic use. Appropriate antibiotic use helps fight antimicrobial resistance and ensures these life-saving drugs will be available for future generations.
Articles
- Antimicrobial resistance explained
- Reducing the risks of antimicrobial resistance
- Tetracycline antibiotics in the environment
- Global report on antimicrobial resistance
- Infection Inspection – citizen science article
- Resistance: When antibiotics don’t work – School Journal article
Webinars
- The science of superbugs – teaching antimicrobial resistance awareness in Aotearoa
- Science for communities with ESR
Media
- Antimicrobial resistance: a major health issue – video
- How bacteria develop resistance to antibiotics – video
- The antibiotic apocalypse explained – YouTube video
- How antibiotic resistance moves directly germ to germ – CDC poster
Image: Poster of how antibiotic resistance spreads. Public domain
Acknowledgment
This interactive was developed in partnership with New Zealand Food Safety.